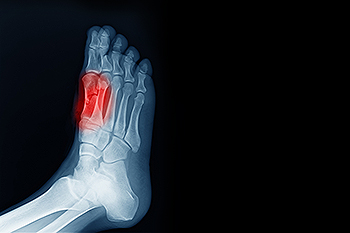
Sesamoiditis is an inflammatory condition that affects the small sesamoid bones beneath the big toe joint, often causing pain at the ball of the foot. These bones act like pulleys, helping the tendons move smoothly and bear the stress of walking, running, or jumping. When repetitive pressure or trauma irritates the area, pain can develop beneath the big toe, especially when bending or pushing off the foot. Symptoms of sesamoiditis include swelling, tenderness, and difficulty walking, sometimes leading to a limping gait to avoid pressure on the forefoot. Although sesamoiditis is not life-threatening, it can disrupt daily activities. A podiatrist can confirm the diagnosis, recommend footwear modifications, and may prescribe custom orthotics to relieve pressure on the joint. Further treatment such as immobilization or surgery may be necessary in severe cases. If you are experiencing pain beneath your big toe, it is suggested that you make an appointment with a podiatrist for a diagnosis and treatment.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact one of our podiatrists of Suncoast Podiatry Associates. Our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Ocala, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

As people age, changes in the feet, toes, and ankles can increase their risk of falling. Reduced joint flexibility, weaker muscles in the lower legs, and diminished sensation in the soles of the feet all contribute to poor balance. Common foot issues, such as bunions, hammertoes, or flat feet, may alter walking patterns and decrease stability. Limited ankle mobility also affects how the body responds to uneven surfaces or sudden shifts in direction. Even dry or thickened skin on the soles can affect grip and lead to slips. A podiatrist can evaluate these factors and provide care that supports balance. Options include suggesting supportive footwear, addressing biomechanical concerns, and prescribing custom orthotics to correct alignment. In some cases, foot or ankle surgery may be needed to correct structural problems that reduce stability. Strengthening the feet and ankles through guided exercises, along with proper foot care, can play an important role in fall prevention. If you are at risk for falling, it is suggested that you schedule an appointment with a podiatrist for an exam and suggestions for maintaining stability.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our podiatrists from Suncoast Podiatry Associates. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Ocala, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Ingrown toenails occur when the edge of a toenail, usually on the big toe, grows into the surrounding skin. This can lead to pain, swelling, and infection. Surgery for ingrown toenails is often recommended when the problem does not improve or keeps coming back. A podiatrist may perform a procedure called a wedge excision, where part of the toenail and the tissue it grows from are removed. In more severe cases, the entire nail may be taken out, termed nail avulsion. A chemical or heat may be used afterward to prevent the nail from growing back, a process known as nail-bed ablation. Another option, Zadek’s procedure, involves removing both the nail and the underlying tissue that causes the nail to regrow. Ingrown toenail surgery is typically done under local anaesthetic and takes about 10 minutes. Infection or toenail regrowth can occur, but many patients experience no such repercussions. If you are experiencing ongoing pain from an ingrown toenail, it is suggested that you schedule an appointment with a podiatrist for an exam, treatment, and possible surgery.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact one of our podiatrists of Suncoast Podiatry Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Ocala, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

